Anterior Implant Esthetics
 The first decision to make is whether the failing tooth is needed for implant site development. The failing tooth may be useful in situations where significant bone loss is associated with the failing tooth but not with adjacent teeth. If one extracts the tooth, the bone level may be more apical relative to the adjacent teeth. This creates a difficult situation for impression taking and implant-supportive maintenance. As plaque accumulates at the implant interface, the inflammation may adversely affect the periodontal status of adjacent teeth.
The first decision to make is whether the failing tooth is needed for implant site development. The failing tooth may be useful in situations where significant bone loss is associated with the failing tooth but not with adjacent teeth. If one extracts the tooth, the bone level may be more apical relative to the adjacent teeth. This creates a difficult situation for impression taking and implant-supportive maintenance. As plaque accumulates at the implant interface, the inflammation may adversely affect the periodontal status of adjacent teeth.  The ideal treatment is to delay the extraction so the failing tooth can be orthodontically extruded. As this is done over the course of six months, the bone and periodontal attachment surrounding the
The ideal treatment is to delay the extraction so the failing tooth can be orthodontically extruded. As this is done over the course of six months, the bone and periodontal attachment surrounding the failing tooth will be coronally
failing tooth will be coronally  positioned to match adjacent bone levels. This provides more ideal bone height and allows the restorative implant platform to be placed at the desired height of 3 to 4 mm subgingivally. This section will focus on situations where the failing tooth needs to be extracted and define key determinants for preserving hard and soft tissue for an optimal implant-supported prosthesis.
positioned to match adjacent bone levels. This provides more ideal bone height and allows the restorative implant platform to be placed at the desired height of 3 to 4 mm subgingivally. This section will focus on situations where the failing tooth needs to be extracted and define key determinants for preserving hard and soft tissue for an optimal implant-supported prosthesis.There are several factors to consider when planning an implant restoration of failed dentition in the esthetic zone. Most often, the esthetic zone involves the maxillary anterior dentition. Although the single-tooth implant-supported restoration appears simple to perform, it is the most challenging in the esthetic zone. One of the initial assessments is determining if the tooth in question is a candidate for immediate implant replacement or a ridge preservation procedure.
The following checklist of nine issues will be discussed.
* Assessment of patient expectations;
* Assessment of gingival display;
* Gingival thickness;
* Papilla presence or absence;
* Morphology of adjacent teeth (crown-to-root ratio);
* Size and shape of contact areas of adjacent teeth;
* Available bone height;
* Available bone width; and
* Studies appropriate for final decision making.




Clinical Considerations for Increasing the Esthetic for Anterior Single-tooth Implant Restorations
1. Bone volume-quality and contour
2. Proximity of anatomical structures
3. Gingival morphology-facial and interproximal
4. Periodontal prognosis of adjacent teeth
5. Mesiodistal width of edentulous space
6. Interocclusal space
7. Implant size and site
8. Custom provisional prosthesis and abutment
9. Oral hygiene, etc.




1 Comments:
Factors affecting the esthetic outcome include:
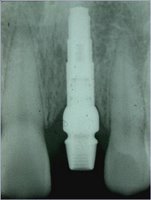
1 - Implant placement: Accurate use of the surgical stent guides the placement of the implant in three different main directions — apico-occlusal, or mesio-distal, or labio-palatal. Each implant should be positioned properly in all three directions. The implant orientation in the alveolar ridge dictates the emergence profile of the tooth to be replaced.
2 - Implant size: Selecting the proper implant size in relation to the size of the missing tooth is a valid rule. In other words, the more the similarity between the diameter of the implant and the diameter of the missing tooth at the bony crest, the greater the esthetic outcome.
3 - Soft tissue profiling: Creation of a soft tissue contour with intact papillae and a gingival outline that is harmonious with the gingival silhouette of the adjacent dentition is the most difficult factor in achieving an optimal esthetic result. Mismanagement of the soft tissue often results in esthetically unacceptable restorations, and such situations are difficult to correct.
3A - Standard operative techniques: The basic principles of the flap reflection, tissue handling and wound closure should be considered in order to prevent post operative complications.
3B - Second stage surgery: An important step in obtaining a soft tissue topography around the implant, making the incisions exclusively in the attached tissues definitely decreases scarring. Transposing the palatal keratinized tissues labially also enhances the emergence contour.
3C - Soft tissue grafting: There are numerous methods to increase the attached tissues or to modify the gingival contour, such as: free gingival grafting ; subepithelial (connective tissue grafting); and coronally repositioning flaps.
3D - Papilla reconstruction: Reconstruction of the interdental papilla is a very unpredictable application in the oral cavity. There are many ways to regenerate the papilla, but none of them provide a reasonable percentage of success.
3E - Gingival recontouring techniques: Techniques can be used to reshape the gingival tissues provided that there are enough keratinized tissue.For example, electro-surgery is utilized to remove scarring and the gingivoplasty by using a diamond bur to remove the excess tissue.
4 - Bone grafting considerations: In the past available bone often dictated placement of implants in areas such as the anterior mandible5. These days prosthetic requirements dictate, to a great extent, the precise placement of the dental implants.
Advancements in the manufacturing of the bone substitutes, the bio-compatibility of the grafting materials, the extended knowledge of bone physiology, and a wider variety of GTR materials, are all factors making the bone grafting techniques more predictable. Therefore, implant placement is now prosthetically driven.
5 - Prosthetic considerations: There is a consensus that prosthetic restoration is the ultimate objective of implant procedures. Each potential implant site should be considered from the perspective of achieving the optimal restoration.
The are many different factors affecting the prosthodontic phase, including:
• healing abutments and their influence to create the gingival collar
• the abutment connection
• the shape of the abutments (e.g. angled abutments, anatomical abutments)
• the color of abutments
• temporary abutments.
The provisional stage of the treatment is another important factor that influences the emergence profile. It creates the papilla or the papillary illusion, etc., resulting in the final restoration.
Finally, each step of the treatment should be managed carefully in order to obtain the desired esthetic outcome, which will satisfy both the patient and the dentist.
Post a Comment
<< Home