Immediate Loading Protocols ( Dr. Balshi on OsseoNews Blog's Interview ) Part I~IV
 Dr. Thomas Balshi and Dr. Glenn Wolfinger have established The Institute for Facial Esthetics in Fort Washington, Pennsylvania. They are Diplomates of the American Board of Prosthodontics and also place all their implants. They have developed surgical and prosthetic protocols for the Teeth-in-an-Hour and Teeth-in-a-Day paradigms. Their web site is: http://dentalimplants-usa.com/. Dr. Balshi has taken time out of his busy schedule to grant an interview to Osseonews.com.
Dr. Thomas Balshi and Dr. Glenn Wolfinger have established The Institute for Facial Esthetics in Fort Washington, Pennsylvania. They are Diplomates of the American Board of Prosthodontics and also place all their implants. They have developed surgical and prosthetic protocols for the Teeth-in-an-Hour and Teeth-in-a-Day paradigms. Their web site is: http://dentalimplants-usa.com/. Dr. Balshi has taken time out of his busy schedule to grant an interview to Osseonews.com.Interview conducted by Gary J. Kaplowitz, DDS, MA, MEd, ABGD
Comment on this interview by visiting the OsseoNews Blog
OsseoNews (ON): Could you present an overview of the immediate loading protocols that you and Dr. Wolfinger have developed and are utilizing at the Institute of Facial Esthetics.
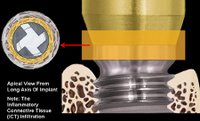
Dr. Balshi: There are several basic concepts that distinguish our protocols from the traditional approach to implant placement and restoration. In the first place, we utilize an immediate loading approach where we place the implants and subject them to loading on the day of surgery. This is our standard operating procedure in contradiction to the traditional placement followed by a waiting period where the implant fixture is undisturbed and undergoes osseointegration. We have been collecting data over two decades and have firmly established that our protocol produces a very high rate of success over the long term.
ON: Could you explain how you have encorporated computer software into your protocols.
Dr. Balshi: We make a CT scan of the patient to generate a three dimensional virtual replication of the bone, soft tissue and alignment of teeth. We feed this data into our software program to generate a surgical guide, which selects the most advantageous implant sites and angulations. The surgical guide will have three guide pins, which will securely stabilize the guide stent during the drilling and placement of the implants. The stent will first be used as a guide to drill a hole for each of the guide pins. The guide pins will then be inserted through the stent and into the bone. The advantage of this technique is that the drilling and placement of the implants is very precise and accurate. The implants end up exactly where you want them, at the desired angulation and the desired occlusogingival height.
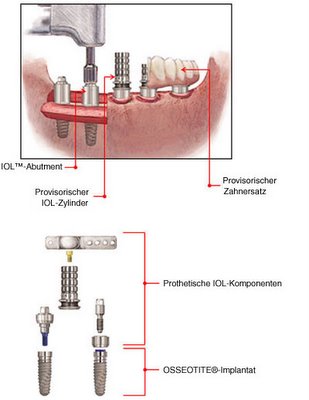
ON: How do you generate the prosthesis?
Dr. Balshi: The prosthesis is generated by the software program based on the data from bone, soft tissue and alignment of teeth. We do a CT scan of the patient at the proper vertical dimension of occlusion in centric relation position.
ON: What if the patient is already wearing removable partial dentures or complete dentures?
Dr. Balshi: We scan the patient wearing the removable dentures. We do a second scan of the removable dentures alone. All of this information that we collect enables our software program to generate a fixed-detachable partial or complete denture that will fit the abutments torqued into the implant fixtures.
ON: The permanent abutments then are also torqued down at the time of implant placement?
Dr. Balshi: The permanent abutments are torqued down permanently at the time of implant placement. They are not removed after they have been torqued down. The final form and orientation of the abutments is established at the time of implant placement.
ON: The CT scan and software program provide accurate enough data to produce a prosthesis that precisely fits the abutments?
Dr. Balshi: The prosthesis fits the abutments with great precision. The prosthesis is then inserted with screw retention.
Log back onto osseonews.com next week for Part II of our interview with Dr. Balshi.
Comment on this interview by visiting the OsseoNews Blog
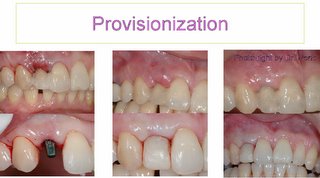
 Case present by Perio: Immediate loading with provisional restoration after Molar implant insertion@
Case present by Perio: Immediate loading with provisional restoration after Molar implant insertion@ 




Dr. Thomas Balshi on Immediate Loading Protocols :Part II>>>
Determining Primary Stability :Part III of IV