Forced Orthodontic Eruption (FOE) before Dental Implantation
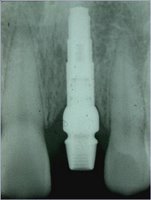
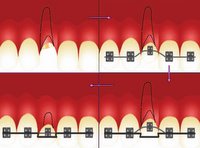 The treatment of esthetic areas with dental implants represents a new challenge for the clinician. Placementof a single-unit implant is indicated for fractured or periodontally compromised teeth. In 1993, a modification ofthe forced eruption technique, called “orthodontic extrusive remodelling,” was proposed as a way to augment both soft- and hard-tissue profiles at potential implant sites. This case report describes augmentation of the coronal softand hard tissues around the teeth with severe periodontal destruction , which was achieved by forced orthodontic extrusion before implant placement. This technique may be used to improve primary anchorage of a dental implant, fill the alveolar socket with bone, preserve interdental bone height and increase the amount of attached gingiva.
The treatment of esthetic areas with dental implants represents a new challenge for the clinician. Placementof a single-unit implant is indicated for fractured or periodontally compromised teeth. In 1993, a modification ofthe forced eruption technique, called “orthodontic extrusive remodelling,” was proposed as a way to augment both soft- and hard-tissue profiles at potential implant sites. This case report describes augmentation of the coronal softand hard tissues around the teeth with severe periodontal destruction , which was achieved by forced orthodontic extrusion before implant placement. This technique may be used to improve primary anchorage of a dental implant, fill the alveolar socket with bone, preserve interdental bone height and increase the amount of attached gingiva.An approach to soft- and hard-tissue augmentation is forced orthodontic eruption (FOE). As first described by Heithersay and Ingber, this technique is based on osteophysiologic and orthodontic principles. It has been usedf requently because of its demonstrated advantages, including correction of isolated infrabony defects, repositioning ofthe gingival margin and clinical lengthening of thecrown.
Clinical Case Report by Perio: (FOE by Dr. Tsai)






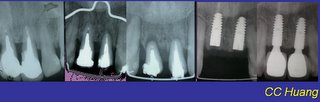
@Buccal and coronal bone augmentation using forced eruption and buccal root torque( Int J Periodontics Restorative Dent. 2003 Dec;23(6):585-91.)
*Multidisciplinary Treatment Approach for Enhancement of Implant Esthetics(Dr. Wang 2004)