Dental Implant Fracture: a complication of treatment with dental implants
 Dental implants are a functional and esthetic solution to partial and total edentulism. The initial success rate of this treatment modality is 90-95%. But, that treatment modality is not free of complications. One of the rare complications yet, with severe clinical results is fracture of dental implants. The current literature review (Biomaterials. 2002 Jun;23(12):2459-65)presents the various causative factors that may lead to implant fracture. Implant failures may be sorted into groups by the timing of their appearance, or by the origin of failure. Fractures belong to the group of late complications, caused by a biomechanical overload.
Dental implants are a functional and esthetic solution to partial and total edentulism. The initial success rate of this treatment modality is 90-95%. But, that treatment modality is not free of complications. One of the rare complications yet, with severe clinical results is fracture of dental implants. The current literature review (Biomaterials. 2002 Jun;23(12):2459-65)presents the various causative factors that may lead to implant fracture. Implant failures may be sorted into groups by the timing of their appearance, or by the origin of failure. Fractures belong to the group of late complications, caused by a biomechanical overload.  Overload may be caused by inappropriate seat of the superstructure, in-line arrangement of the implants, leverage, heavy occlusal forces (bruxing, clenching), location of the implant and the size of the implant or metal fatigue. Good clinical examinations and correct treatment plans may reduce the risk of implant fracture.
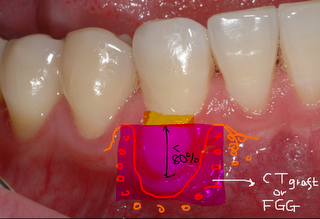
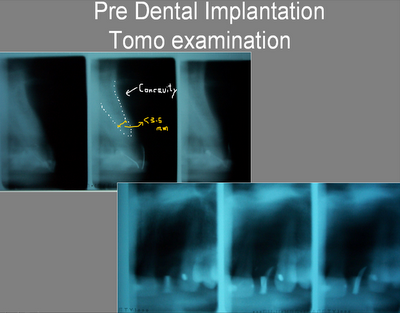
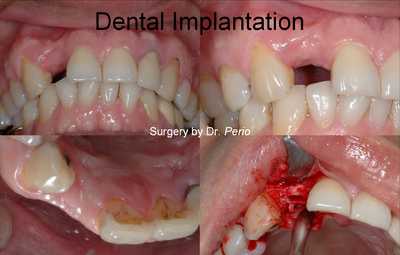
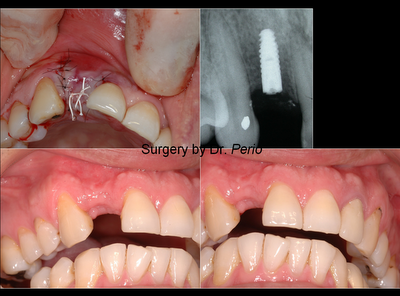
Overload may be caused by inappropriate seat of the superstructure, in-line arrangement of the implants, leverage, heavy occlusal forces (bruxing, clenching), location of the implant and the size of the implant or metal fatigue. Good clinical examinations and correct treatment plans may reduce the risk of implant fracture.*A Case Report for Fractured Implant Removal:

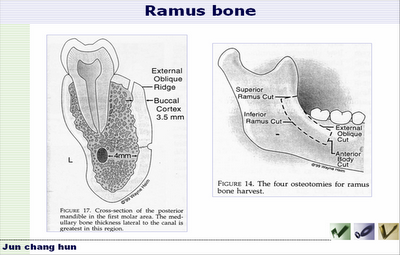
 >>Trephine to remove the fractured implant
>>Trephine to remove the fractured implant

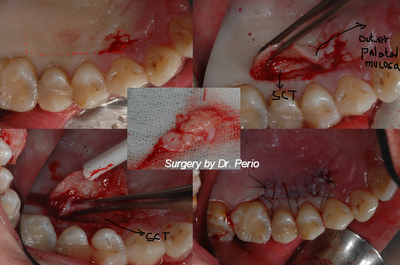
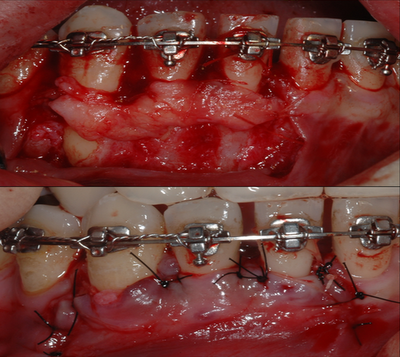
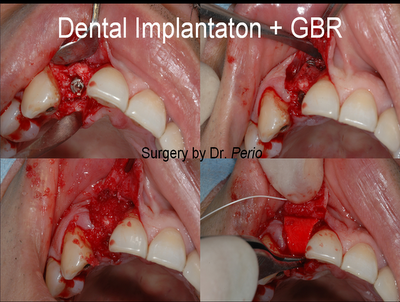
 *New larger implant with bone graft into the old implant site>>
*New larger implant with bone graft into the old implant site>>
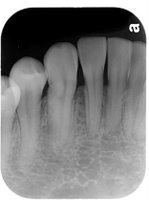
@Final Restoration:( after 6 months later from reimplantation!)
Labels: implant complications