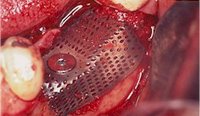
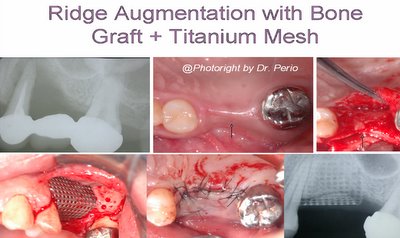
Localized ridge augmentation using titanium mesh
A configured titanium mesh (CTM) is served as a mechanical and biologic device for restoring a vertically defected/resorbed alveolar ridge.

Vertical ridge augmentation using xenogenic material supported by a configured titanium mesh: clinicohistopathologic and histochemical study
Artzi Z, Dayan D, Alpern Y, Nemcovsky CE.
Int J Oral Maxillofac Implants, Vol. 18, No.3, pp:440-446,2003.
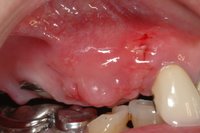
MATERIALS AND METHODS: The study comprised 10 severely resorbed sites in 10 patients. Pre- and post-operative ridge measurements were taken with reference to the neighboring teeth and supporting screw head base of the CTM. Bio-Oss® served as the augmentation filler material. The metal mesh was removed after 9 months. Subsequently, root-form, screw-type implants were placed. During the implant placement phase, cylindric bone samples were retrieved from the augmented area for histopathologic and histochemical examination.
RESULTS: Upon soft tissue reflection and before augmentation, defect height, as recorded by a periodontal probe along the main threads exposed on the support screw, was between 5 and 8 mm (average 6.4 mm; SD +/- 1.17). At 9 months after augmentation, during the implant placement phase, the defect height was between 0 and 2 mm (average 1.2 mm; SD +/- 0.63). Differences were statistically significant (P < .001). Bone height gain was between 4 and 6 mm (average 5.2 mm, SD +/- 0.79), which gave an average bone fill of 81.2% (SD +/- 7.98). Polarizing microscopic examination of sections stained with Picrosirius red showed a gradual increase in new lamellar bone from coronal to apical cuts, reaching the highest area percentage in the deep apical zone. DISCUSSION: At 9 months postaugmentation using the CTM surgical technique, the quality and quantity of the newly established hard tissue appeared to be different in the coronal versus apical areas of the restored alveolar ridge.
CONCLUSION: Although at 9 months postoperatively, the augmented alveolar ridge had different bone content, clinicohistochemical results demonstrated that this surgical technique could be a successful.
A Titanium Mesh is stabilized by screwing it onto one of the implants. Bone graft material is deposited under the Mesh and around the implants. The Mesh is then formed into the desired ridge shape and the gum tissue pulled over the entire site and sutured together. The Mesh will protect the graft from chewing forces while still allowing blood flow through the opening areas. Because the graft site will remain below the gum tissue during the initial growth period, it will also be protected from bacteria. The Mesh will remain under the gum tissue TEMPORARILY for approximately six weeks to a six months period while bone grows into the space under the Mesh.
Free Article>>>Three-Dimensional Bone Reconstruction in thePosterior Mandible Using DFDBA in a BiologicCarrier Matrix and Titanium Mesh
@@Clinical Application by Dr Perio


@Titanium Membranes in Prevention of Alveolar Collapse After Tooth Extraction. Implant Dentistry. 15(1):53-61, 2006. Pinho et al.
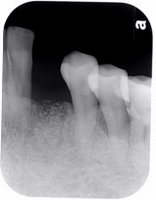
Background and Purpose: The resorption of alveolar bone following tooth extraction results in a narrowing and shortening of the residual ridge, which leads to esthetic and restorative problems, and reduces the bone volume available for implant therapy. The aim of this study was to evaluate the prevention of alveolar collapse after tooth extraction, using titanium membrane (Frios Boneshield; DENTSPLY Friadent, Mannheim, Germany), associated (or not) with autologous bone graft.
Materials and Methods: A total of 10 nonsmoking healthy subjects, ranging from 35 to 60 years old, were selected for this study. Each patient had a minimum of 2 uni-radicular periodontally hopeless teeth, which were scheduled for extraction. After the procedure, 2 titanium pins were fixed on the vestibular bone surfaces that were used as references for the initial measures (depth, width, and height) of the socket. Of the sockets,1 was randomly chosen to be filled with autologous bone graft (test) removed from superior maxillary tuber, and the other one did not receive the graft (control). A titanium membrane was adapted and fixed, covering the sockets, which remained for at least 10 weeks. After a 6-month healing, the final measures were performed.
Results: There was exposure of the membrane in 5 of the 10 treated subjects. Average bone filling (+/-standard deviation) among the 10 subjects was 8.80 +/- 2.93 mm (range 4-13) in the control group and 8.40 +/- 3.35 mm (range 4-13) in the test group. Average bone loss in width in both group was 1.40 +/- 1.97 mm (range -4-1) in the control group and 1.40 +/- 0.98 mm (range -4-0) in the test group. There was no significant statistical difference between groups considering the evaluated standards.
Conclusion: The use of titanium membrane, alone or in association with autogenous bone, favored the prevention of alveolar ridge after tooth extraction. This membrane seems to be a possible and safe alternative to other nonresorbable membranes when the prevention of alveolar ridge resorption is the objective.
@ Question from Dr. Perio
Is it necessary to put a resorbable membrane over the Titanium mesh + bone grafting for GBR before dental implantation? Comments...