Surgical extrusion technique for clinical crown lengthening
Int J Periodontics Restorative Dent. 2004 Oct;24(5):412-21.
Surgical extrusion technique for clinical crown lengthening: report of three cases.
Kim CS, Choi SH, Chai JK, Kim CK, Cho KS.
Department of Periodontology, Research Institute for Periodontal Regeneration, Oral Science Research Center, College of Dentistry, Yonsei University, Seodaemun-Gu, Seoul, Korea.
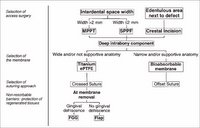
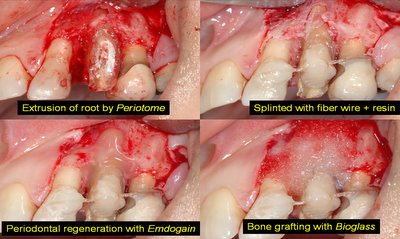
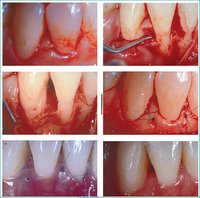
Although a number of techniques have been proposed for clinical crown lengthening procedures, all have some limitation in terms of function and esthetics. This report presents the clinical and radiographic results of a surgical extrusion technique for clinical crown lengthening. Atraumatic surgical extrusion using a specially designed instrument (Periotome) was performed in three cases in which it was expected that extensive resective osseous surgery would have to be used for crown lengthening. Full-thickness mucoperiosteal flaps were raised both labially and palatally. The tooth was carefully luxated and extruded to the desired position without damaging the marginal bone area or root apex. No rigid splint was applied. Clinical examinations performed for more than 1 year after surgery revealed probing depths < or =" 3">@ Clinical procedure for CLP with surgical extrusion

 @ Orthodontic Extrusion for CLP (PDF from U. Ohio)
@ Orthodontic Extrusion for CLP (PDF from U. Ohio)



















 to the alveolar crest.
to the alveolar crest.