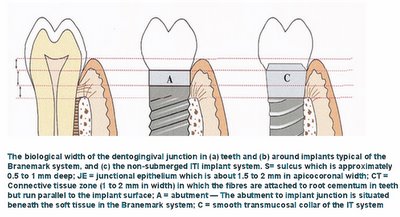
*An osseointegrated implant restoration may closely resemble a natural tooth.However, the absence of a periodontal ligament and connective tissue attachment via cementum, results in fundamental differences in the adaptation of the implant to occlusal forces, and the structure of the gingival cuff.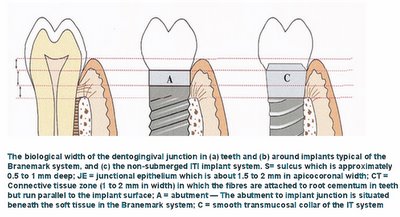

@ The Outlines from Keynote speech by Dr.
Berglundh on
EAO05'
Topic:What determines the biological width at implants?Integrated esthetics – a biological and biomechanical approach
• Definition of “Biological width”
• Clinical soft tissue dimensions
• True soft tissue dimensions
• Soft tissue integration to different materials
Dimensions and relations of the dentoginigval junction in humans (1)
Sample:
Human autopsy specimens (Orban's and Kronfei's collections) exhibiting varying degree of periodontal tissue breakdown
Examination:
Histometric assessment of
Epithelial attachment
Connective tissue attachment
Dimensions and relations of the dentoginigval junction in humans (2)
Normal
Moderate breakdown
Advanced breakdown
Dimensions and relations of the dentoginigval junction in humans (3)
Results;
Epithelial attachment varied:
1.4 mm (normal)
0.8 mm (moderate breakdown)
0.7 mm (advanced breakdown)
CT attachment was stable:
1.1 mm
And did not vary with degree of bone loss
Dimensions and relations of the dentoginigval junction in humans (4)
Conclusion:
The biological width of soft tissue attachment is about 2.5 mm and includes 1.5 mm epithelium and 1 mm connective tissue.
Clinical soft tissue dimensions
Implant supported single tooth replacements compared to contra-lateral natural teeth.
Probing >>
Chang et al 1999Dimensions of peri-implant mucosa at evaluation of maxillary anterior single implant in man.
Bone sounding>>
Kan 2003The height of the mucosa at single implants and teeth
Implant Teeth
facial aspect
Probing: 3 mm 2 mm
Sounding: 4 mm 3 mm
proximal aspects
Probing: 4 mm 3 mm
Sounding: 5-6 mm 4 mm
The biological width: 2.5 mm (Gargiulo et al 1961)
PPD under estimates
Sounding over estimates
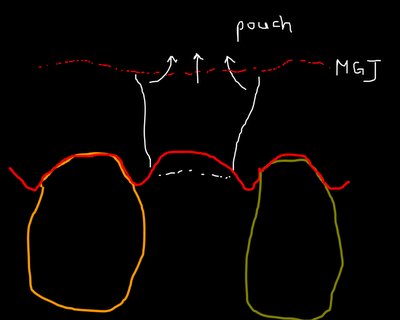
“Biological width” is not synonymous with Probing Pocket Depth or with SoundingTrue soft tissue dimensions
The soft tissue barrier at implant and teeth (Berglundh et al 1991)
PM/GM~aJE= 2.14 / 2.05 mm
aJE~B= 1.66 / 1.12 mm
The mucosal at implants is comprised of a 2 mm long barrier epithelium and a 1-1.5 mm zone of “connective tissue integration”.
The “connective tissue integration” zone is characterized by absence of blood vessels and a large number of fibroblasts interposed between thin collagen fibers.
Dimensions of the periimplant mucosa (
B & L 1996)
3 beagles dogs
3 months:
Flap adaptation and suturing
Test OE=2 mm
Control OE=4 mm
6 months:
Test
PM~aJE 2.0
aJE~B 1.3
Control
PM~aJE 2.1
aJE~B 1.8
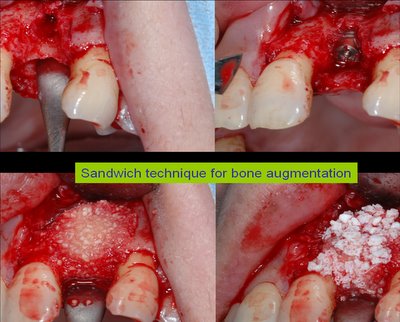
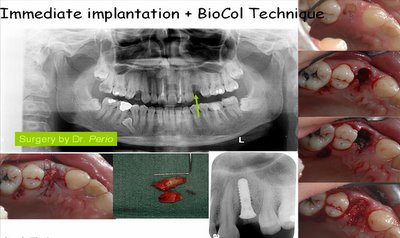
A minimum width of the periimplant mucosa is required and bone resorption may take place to allow a proper mucosal attachment to form.
Morphogenesis of the mucosal attachment at implants (Berglundh et al 2006)
The soft tissue dimension – the biological width – at implant was established after 6 wks following Sx
How to preserve the marginal bone and avoid soft tissue recession ?
Respect the biological wwidth
Soft tissue integration to different abutment materials (Wennstom 2006)
Abutment shift (1 month after implant surgery)
Control abutment: Ti (c.p. Ti)
Test abutment: Direct (c.p. Ti)
Conclusions
The soft tissue dimensions were similar at implant abutment made of c.p. Titantium, ZrO2, based Ceramic and Au/Pt alloy
The connective tissue interface at Au/Pt alloy abutment contained lower amount of collagen and larger portions of leukocytes than that at abutment made of Ti and ZrO2
@ A review article of "teeth and implant" on BJD@The effect of subcrestal placement of the polished surface of implants on marginal soft and hard tissues-a retrospective clinical study*** On Line Internet Course: Biological Width by Dr. S. Robert Davidoff@ Abstracts of Biological Width for Dental Implants$$$ The biological aspects of the soft tissue – Titanium implant interface (PDF)


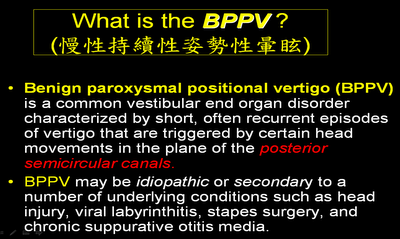
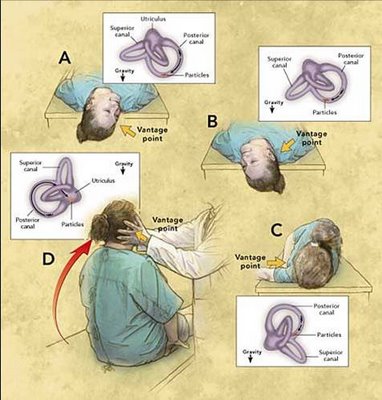
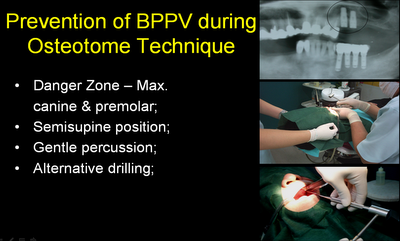 @ Dignosis and Therapy for BPPV:
@ Dignosis and Therapy for BPPV: